
This blog piece is a book chapter written by David Nutt from a book on addiction, targeted at Sixth Form and secondary school students
What is addiction?
Addiction is a behavioural pattern that certain people experience as a result of taking part in certain activities such as gambling or taking some drugs. Addiction, particularly to some drugs such as heroin alcohol and cocaine is a serious mental illness with survival rates less than those for many cancers (ref). Its main feature is that the person finds they are compelled to keep on doing the behaviour despite the fact that they know it is bringing harm to them and their friends and families. They often dislike doing it but find something compels them to keep on doing it. In fact the word addiction means “enslaved” which well explains the sense of being trapped in unwanted behaviours that addicts experience. Often there is a sense of craving for the drug or behaviour that keeps the addict doing it, and when they are able to stop this, craving can become intense so lead to relapse. Also in many cases a withdrawal reaction from stopping the behaviour is seen. This is most obvious with drugs, so that suddenly stopping alcohol addiction can lead to severe medical problems such as seizures (fits) and delirium (confusion with hallucinations).
Why do people become addicted?
There are three necessary elements that determine why drug addiction occurs, shown below in Fig 1

Figure 1: Triangulating addiction
Social factors
These relate to the fact that the addictive drug or behaviour (e.g. gambling) most be available or accessible. In the case of drugs, if the drug is not present in society then people will not easily be able to use it so they can’t get addicted to it. Where gambling is banned fewer people take part so there is less addiction to it. For example in most Islamic countries alcohol is banned and rates of alcohol addiction are very much lower than in countries such as the UK where it is freely available and actively marketed. However banning a drug or activity doesn’t completely prevent addiction as illegal markets often develop. Even in Islamic countries a significant number of people are addicted to alcohol. And in the UK, despite the drugs being “illegal” there are over 300,000 people addicted to drugs such as heroin and crack cocaine. () This tells us that the desire to take a drug or gamble can be so powerful that it overcomes the threat introduced of breaking the law.
Other important social factors are the costs of drugs or gambling and fashion. In general the cheaper the drug the more people will try and so more will be at risk of addiction. In the last twenty years we have seen the real price of alcohol fall and this has lead to a big increase in drinking.
Fashion dictates a lot of human behaviour and when some drugs have become fashionable then use has increased; again alcohol is a good example as advertising of this drug is allowed so it has been made very fashionable. Cocaine use in the business and banking sector became fashionable in the 2000s and may have contributed to the banking crash!
Personal biological factors:
Most people who use alcohol and other drugs or try gambling do not get addicted. This tells us that there must be some factors in the individual that make some people more vulnerable to addiction. These can be due to differences in brain function or in the way different people’s bodies deal with drugs. The most important of these are shown in Fig 2.
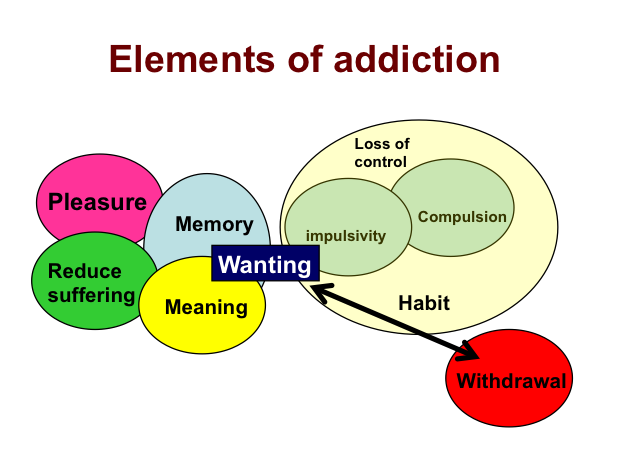
Figure 2: The many elements of addiction
A common misunderstanding is that all drug use is driven by pleasure. This is true for some people and drugs like heroin produce such profound changes in the way people feel that they can quickly lead to addiction. But some people are vulnerable to drug addiction because they use drugs to reduce suffering. For example, people who use alcohol or drugs to deal with mental health problems such as anxiety or depression instead of seeking proper help have a higher risk of addiction. Similarly some impulsive people find it hard to stop using drugs once they have started. This is particularly difficult for those with attentional deficit problems such as attention-deficit hyperactivity disorder (ADHD) who use stimulants as these can improve their attentional problems i.e. effectively self-medicating their underlying problems.
For some people drugs give meaning to their life – as a psychiatrist treating addiction I have often come across patients who say that they only feel “right” when on drugs. The Oscar winning actress Tatum O’Neal who married and had two children by the top tennis player John McEnroe famously said the only time she felt whole was when on heroin. This shows how a drug can be more significant than fame, wealth, success or even parenthood and explains why addicts find stopping drug use can be so very difficult.
Factors that perpetuate addiction
Whatever the reasons people use drugs the effects are often profound and become some of the most powerful memories that individuals ever have. In addiction these memories lead to drug wanting (craving) that can take over a persons life to the extent that they will put their addiction before their jobs and families. Often the addiction process can become almost automatic, people find themselves using drugs despite desperately wanting not to. In this regard addiction behaviour is like that seen in forms of obsessive-compulsive disorder where extreme behavioural habits control peoples lives. For others the fear of drug withdrawal can be so overpowering that they are too scared to stop. The images of heroin withdrawal shown in the film Trainspotting are a good example of this.
Often peoples drugs use starts because of the pleasure drugs give but over time as addiction develops then the driver to continue use is to prevent withdrawal; at this stage all pleasure form the drug can be lost. That addiction can change peoples’ whole lives and fundamental behavioural attributes so profoundly tells us that drugs affect core brain processes and is a form of mental illness.
Addiction and the brain
We are now beginning to understand the brain factors that underpin addiction.
We also know a great deal about the targets that drugs act on in the brain and where in the brain drugs and gambling have their actions. In turns out that there are many different targets of drugs that can cause addiction. These are shown in Table 1.
Drugs are classified by their pharmacological actions, i.e. by the neurotransmitter targets in the brain that they work on. Opioids include heroin morphine methadone and buprenorphine (Subutex) and all these act at the mu opioid receptor. This receptor exists to allow endorphins – the brain’s natural pain killer- to act when needed, so opioid drugs mimic this endogenous neurotransmitter. Opioid drugs have stronger actions than the natural endorphins and this leads to problems such as accidental death by respiratory depression from opioids (particularly when used via the intravenous route). Tolerance develops to this action and also to the pleasurable effects so requiring massive does escalation in regular users.
There is growing evidence that the endogenous opioid system is involved in addiction to drugs such as alcohol and cocaine as well as heroin and both stimulants and alcohol can be shown to lead to endorphin release in human brain. Also levels of mu opioid receptors are increased in these addictions suggesting an underlying dysfunction of the system.
Other drugs of addiction act on different neurotransmitter processes in the brain. Stimulants include drugs such as cocaine and crack cocaine, amphetamines and newer drugs such as mephedrone. These act to enhance the effects of the neurotransmitter dopamine. Dopamine that has a major role in directing motivation and facilitating motivated behaviour. Also dopamine systems can undergo a process of sensitization whereby repeated release leads to enhanced effect rather than tolerance. This is one factor in why addiction to stimulants develops.
Nicotine (as tobacco) is a mild stimulant that is not pleasurable to start with due to the unpleasantness of inhaling burning plant material. That so many people smoke despite this initiation challenge shows the power that peer-pressure and fashion has to drive drug use. Once people get over this phase then tobacco becomes the most addictive drug because people continue to use to prevent the withdrawal reactions of irritability and depression that are so common.
Sedative drugs include alcohol, benzodiazepines and GHB. These can activate people as a dose begins to have its effects to switch of the parts of the brain that inhibit behaviour (disinhibition), but later on at high doses they can cause serious sedation that may result in death from stopping breathing. Their main target is the brain GABA-A receptor, which provides the main calming influence in the brain. By activating this system alcohol and other sedative drugs relax people and are almost universally used to reduce anxiety in social situations such as parties. However tolerance develops so that more is needed to give the same effects and the changes underlying tolerance then lead to dependence and withdrawal. Social anxiety is the leading cause of alcohol addiction in young men with up to 25% of male alcoholics drinking to overcome their fear of social situations particularly when meeting strangers they feel attracted to (refs).
Cannabis acts on so-called cannabis CB1 receptors in the brain. These are the targets of natural neurotransmitters such as anandamide that are made on demand in the brain during activities such as memory and seizures. The endogenous cannabinoids have a major role in synaptic activity and memory formation and, in ways we don’t fully understand, cannabis mimics some of these but blocks others.
MDMA and psychedelic drugs act on the serotonin (5HT) systems in the brain. MDMA releases serotonin in parts of the brain that control emotions such as the amygdala and this explains why it reduces anxiety and makes people more empathetic. Psychedelics activate a particular serotonin receptor (5HT2A) that is highly localised in the cerebral cortex and so profoundly alter integration of cortical functions. Serotonin-acting drugs tend not to be addictive, and are usually used quite intermittently, maybe only a few times in a lifetime with psychedelics. There is growing evidence that psychedelics may instead have anti-addiction properties.
Most of the current treatments we have for addictive drugs are derived from other drugs that act on the receptors the drugs target. So methadone and buprenorphine are less-rewarding versions of heroin that are prescribed to help heroin addicts stop injecting heroin and engage in so-called substitution or maintenance treatment. This means that they can stop engaging in criminal behaviour to get money to buy drugs and also reduces markedly the risk of HIV spread. Antagonists to the mu opioid receptor such as naltrexone can also be used but as they are not pleasure-giving addicts are less inclined to stick with treatment.
The concept of substitution treatment is a powerful one that has been proven to work for alcohol (sodium oxybate, baclofen) nicotine (varenicline) as a prelude to giving up the drug use altogether. Antagonist treatments in theory could also be used for benzodiazepine addiction (flumazenil) and cannabis (rimonabant).
Another approach is to find treatments that can alter the impact of drug use e.g. to reduce craving e.g. acamprosate for alcoholism and bupropion for smoking. A recent novel development is the concept of a “drinking regulator” based on the finding that the opioid antagonist nalmefene can reduce the loss of control of behaviour that alcohol produces in some people and that leads to bingeing.

Table 1: The neurotransmitter targets of drugs
Treatments in brackets are theoretically effective though not yet in current use
Drug factors
In Table 1 above the sites of action of drugs on brain neurotransmitter systems are outlined. However not all drugs that work on these systems are addictive and even if they are the degree of addictiveness (often called abuse potential) can vary greatly. For example both heroin and codeine act on the same mu opioid receptor as both are converted to another opioid – morphine – before they work in the brain. However heroin is much more addictive because it gets in the brain faster – and the speed of brain entry is a major factor in how “high” a drug makes a user. Heroin is even more addictive when made into a soluble salt and then injected iv as it gets into the brain even faster. Some opioid drugs e.g. loperamide are more potent than heroin yet don’t give a “high” at all as they are rapidly pumped out of the brain. This means that they can safely be used to stop travellers’ diarrhoea without having any abuse potential.
Over the centuries humans have made efforts to change drugs to speed up their entry into the brain. A classic example is cocaine. This is the product of the coca plant that grows in the Andes Mountains in South America. For thousands of years the native inhabitants used to chew the leaf or make a tea from them to improve their ability to work at high mountain altitude. They suffered no ill-effects and did not become addicted. However once the active ingredient – cocaine – was identified, purified and brought into medical practice as the hydrochloride salt (cocaine HCl or cocaine powder) addiction to it developed through snorting and occasionally injecting. In the second half of the last century practical ways of making cocaine as a base were discovered. This led to the rapid use of base cocaine (Crack or free-base) by smoking. The surface area of the lungs is so large that smoking a drug gives almost the same rate of brain entry as injecting it intravenously. Crack is therefore significantly more addictive than snorted powder cocaine. Similarly, the freebase of methyl-amphetamine (crystal meth) can be smoked and this makes it more addictive than swallowed methyl-amphetamine or amphetamine sulphate tablets.
To reduce their abuse potential some medicinal drugs are put in formulations that mean they get into the brain more slowly. Sadly, some users work out ways to get the active drug out of the formulation do they can inject or snort it, so getting faster and stronger effects. Intravenous injection is the most dangerous way to use drugs because it maximises the immediate adverse effects and also when needles are shared leads to viral infections such as hepatitis C and HIV.
Similar factors affect the addictiveness of gambling. Many betting machines are programmed to give lots of “near misses” and these make the gamblers feel that they are likely to win the next time so they continue to play even though the know the odds haven’t actually changed in their favour.
Using a combination of animal studies and human imaging experiments it has proved possible to work out there are four main brain circuits involved in addiction. These are shown in Fig 3 where each is colour-coded.
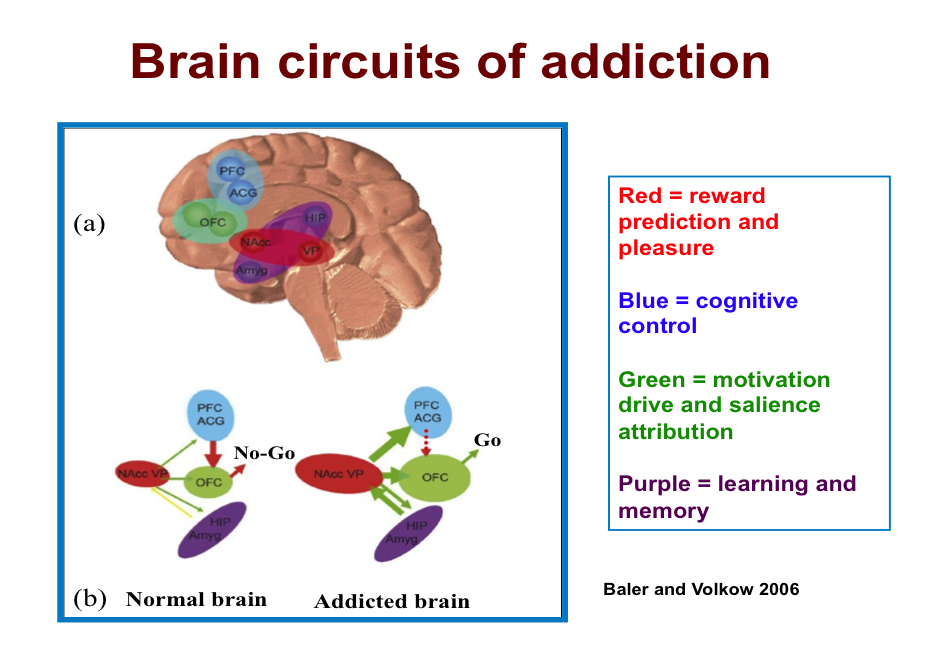
Figure 3: The brain circuits of addiction
The four circuits each have different functions. The red ones are those involved in reward and pleasure specifically the dopamine pathway from the ventral tegmental area (VTA) to the nucleus accumbens (NAcc). This responds to the value of drugs or wining at gambling and encodes particularly good effects so that the behaviour leading up to them can be easily repeated. As drugs/gambling becomes more addictive then other dopamine pathways in the striatum become engaged and this leads to the habit element of addiction.
The orbitofrontal (OFC) circuit is responsible for evaluating the salience (value) of a planned addictive behaviour and regulating the motivation to engage in it. It gets input from the NAcc where the more dopamine is released the more the urge to use drugs is experienced.
The memory elements of addiction are held in the purple circuit, which includes the amygdala (Amyg) and the hippocampus (Hip). The amygdala encodes the emotional elements of addiction and the hippocampus the factual aspects such as how much, where to get drugs, who to get them from etc.
The blue circuit is that which holds the other three under cognitive control. It is the top-down regulatory pathway from the prefrontal cortex (PFC) and anterior cingulate gyrus (ACG) that normally prevents any of the other three, especially the OFC from getting out of control (part b). As addiction develops then the normal balance between these centres begins to get distorted. For example the push from the NAcc to the OFC and from the memory circuit to the NAcc increases so increasing the drive to use drugs. Also the top down control from the PFC is weakened perhaps due to increased input from the NAcc so the person is less able to control these urges to use (part c). Eventually the balance between the restraint and go systems breaks down and drug intake or gambling starts again.
Some drugs can directly affect these pathways e.g. stimulants enhance and can sensitize dopamine function. Others may act indirectly e.g. opioids can reduce the ability of the PFC to exert to-down control of impulses to use drugs. Alcohol may do both.
The importance of these neuroscience insights is that they offer a way to explore new approaches to treatment. For example the ability of the PFC to restrain addiction might be enhanced by drug such as modafinil that can enhance cognitive function. It might be possible to erase the memories of addiction using techniques such as recall-extinction under the influence of glutamate-enhancing drugs such as D-cycloserine. Some researchers are investigating if techniques such as deep brain stimulation might help break the obsessive-compulsive pattern of drug use.
Conclusions
Addiction is a serious mental illness that afflicts a proportion of people who take drugs or who gamble. It is a disorder of the brain with a number of treatable causes though social and pharmacological factors play a part. Advances in neuroscience have helped us understand how brain pathways involved in memory motivation and cognition are disturbed in addiction and hopefully will lead to new treatments.

