T21 Findings
Here you can find a top level overview of the findings from our our medical cannabis study, T21,
and access our publications.

Patient Numbers

Primary Conditions

T21 participating Clinics

Characteristics & Formulary
T21 Publications
Medical cannabis for chronic pain in the UK:
a 12-month longitudinal observational study of 1721 individuals
A substantial proportion of individuals with chronic pain may benefit from CBPMs, demonstrating reduced pain scores and prescription opioid use. 6-months may be the optimal trial duration to assess response, and benefits are generally durable among responders.
Data Nuggets
When I first joined T21 in 2022, I was 28 years old and weighed 117kg. I worked; I was going through a major life change; my anxiety was terrible; my pain level with my autoimmune conditions (Raynaud’s syndrome and Rheumatoid Arthritis) was reaching a point of debilitation; my anxiety and inactive lifestyle was contributing to my depressive state. Due to my stressful circumstances, my Raynaud’s was playing havoc – I was experiencing bouts of panniculitis, and this, coupled with the pain of rheumatoid arthritis, meant that I was unable to imagine much of a future for myself. I was not active at all and had no drive for life, other than to go to work and pay my bills.
I reached a point where I knew I needed to seek help, yet “standard” medicine could only offer me anti-anxiety medication and pain relief. Previous treatments included Valium for anxiety, corticosteroids, pain management and therapy. I researched alternative, less addictive medicines which might be able to improve my overall quality of life and help me be more productive. It was at this point that I sought consultation through a medical cannabis dispensary – I was informed about T21 and it turned out that I was eligible to join the study.
A year on from joining T21, I have lost 37kg, my pain is manageable, I am far more active than I thought I would be, my anxiety has lifted, and I am far happier than I have been for several years. My professional and personal lives feel balanced and harmonious. I use my cannabis products according to my needs and so far haven’t experienced any sense of dependency. My cannabis prescription has aided me in living a more productive and fulfilling life. Past treatments aided in treating the symptoms, but they did not create effective change; they were a “band aid” whereas medical cannabis treatment removed the “band aid” and gave me my life back.
I am very grateful to have the opportunity to be part of the study – it was perfect timing and allowed me to really turn my life around. I still have a way to go, but my mental health and autoimmune conditions are manageable. Cannabis medicines have helped me immensely and given me a better quality of life. The clinic team and staff were an incredible aid to me on my journey for which I am extremely grateful. Comparing where I was to where I am today, I have done a complete 180 in just one year.
I consider this experience a “good news story” that I want to share with others. It is a little strange when I think back on how far I’ve come. I hope T21 is as successful for others as it has been for me.
Keri-Anne Gray
In April 2022, we looked at the types of products prescribed at the initial consultation – you can read more about this if you scroll down to our Data Nuggets here.
Expanding on this analysis, we wanted to explore the products that patients with primary conditions falling under different categories have been prescribed at their 3 month follow-up consultation. For the purposes of this analysis the primary condition categories are defined as:
-
Chronic pain conditions: Arthritis, Back and/or Neck Pain, Cancer Related Pain, Complex Regional Pain Syndrome, Ehlers-Danlos Syndromes, Endometriosis, Fibromyalgia, Musculoskeletal Pain, Neuropathic Pain, Other condition that causes Chronic Pain, Palliative Care Pain
-
Psychiatric conditions: Agoraphobia, Attention Deficit Hyperactivity Disorder, Cancer Related Anxiety, Eating Disorders, Generalized Anxiety Disorder, Insomnia, Major Depressive Disorder, Obsessive Compulsive Disorder, Other condition that causes Anxiety, Palliative Care Anxiety, Panic Disorder, Post Traumatic Stress Disorder, Social Anxiety Disorder, Substance Use Disorder
-
Neurological conditions: Autism Spectrum Disorder, Cluster Headaches, Epilepsy, Migraines, Multiple Sclerosis, Parkinson’s Disease, Stroke, Tourette’s Syndrome, Tremors
-
Other conditions: Chronic Fatigue Syndrome, Crohn’s and/or Ulcerative Colitis, Irritable Bowel Syndrome, Restless Legs Syndrome, Other
We wanted to explore what kind of products are prescribed at 3-months based on the primary condition category of the patients.
When patients join the project they are started on a product (or products), then through trial and error and careful titration of dosages they find the suitable products for their condition. At 3 months after treatment initiation, patients would be expected to feel a bit more settled with their prescriptions, so we chose to look at 3-month follow-up data for the purposes of this analysis.
Data on primary condition and products prescribed at 3 months was available for 1623 patients and can be seen in the table below.
The most commonly prescribed category of products across all patient groups was high THC flower, with 80% of all patients being prescribed at least one strain of high THC flower. A higher percentage (91%) of patients with a psychiatric condition were prescribed at least one high THC flower compared to 71% of chronic pain condition patients, 76% neurological condition patients and 75% patients with Other conditions that do not fall under the previous categories.
Balanced oil was the second most commonly prescribed type of product, with 41% of chronic pain patients being prescribed at least one product vs 19% of psychiatric condition patients.
High CBD oil was more commonly prescribed to 11% of both chronic pain and neurological condition patients and only 6% of Other conditions and 2% of psychiatric condition patients.
As the project moves forward, we will continue to explore the categories of products that patients are prescribed and track how these change over time.-
Epilepsy is the fourth most common neurological disorder in the world. It is a brain disorder that causes recurring, unprovoked seizures. Not all seizures are the result of epilepsy. Seizures may relate to a brain injury or a family trait, but often the cause is unknown. Epilepsy affects both sexes and all ages and occurs in all countries and regions of the world[1].
In T21, 29 people have reported Epilepsy as a primary condition and 48 as a secondary condition (77 overall) and the characteristics of these people are shown in the Table below.

Patients who report epilepsy as a primary condition complete the Patient Weighted Quality Of Life In Epilepsy questionnaire (QOLIE-10-P) which consists of three parts (A, B, C). Part A has 10 items which assess feelings, limitations with activities, and quality of life. Part B asks assesses the overall impact of these problems (reported in part A) on the patient’s quality of life in the past four weeks. Finally, part C asks the patient to indicate the areas related to their epilepsy that are most IMPORTANT to them NOW.
By the end of June 2023, 15 epilepsy patients had completed both their initial evaluation (baseline data) as well as their 3 month follow-up. There was a statistically significant (p<.02) decrease in the epilepsy scores of these patients at 3 months with a mean difference of 0.37.
In addition to the QOLIE-10-P patients are asked to report the approximate number of seizures they had in the last three months and to rate the average severity of these seizures as mild, moderate or severe.
After 3 months of medical cannabis treatment, the average number of seizures over the past 3 months had fallen from a mean of 65 to a mean of 21. This change was statistically significant (p<.03) Additionally, the severity of these seizures had been decreased from a mean of 2.4 at the start of treatment to 1.9 at 3 month follow-up (p>.05), indicating a more moderate severity.
Data from T21 suggests that medical cannabis can help reduce both the frequency of seizures for patients with adult epilepsy as well as the severity of them. Given the severe side effects of common antiepileptic medication and the relatively safe profile of medical cannabis, medical cannabis can have an important role in the treatment of epilepsy.[1] Beghi E (2019) The epidemiology of Epilepsy. Neuroepidemiology 54(2): 185–191.
When patients register on T21, they report one primary condition as the main reason for seeking out medical cannabis treatment. They can then report any secondary conditions (also known as comorbidities) and symptoms, such as stress, headaches and muscle spasms, that they may experience.
The figure below shows the 10 most common secondary conditions for T21 patients and the percentage of patients that report each of these comorbidities.

Based on our current data (3766 patients) the most common secondary condition on T21 is Major Depressive Disorder (MDD; commonly referred to as Depression), with 32% of T21 patients reporting co-morbid depression. This is not surprising, as chronic conditions often go hand in hand with depression. It is for this reason that all T21 patients complete the PHQ-9 which assesses mood and levels of depression. If you are interested in the change in mood/depression over time, take a look at our data nugget from Nov 2021 called “Mood” here (scroll down).
The second most common condition is Back and/or neck pain (29%), followed by Stress (26%) and Insomnia (26%). Back and/or neck pain, MDD, Fibromyalgia, Neuropathic pain and arthritis are commonly found to be both primary and secondary conditions.
Comorbid conditions are common; yet are often used as the basis for excluding people from clinical trials. It is possible that results from clinical trials of cannabis may not represent the ‘real world’ cohort of patients seeking medical cannabis. This may also explain the relatively more positive results from observational studies like T21 compared with results from clinical trials which are often showing smaller improvements in health. Also, it is important to note that as data continue to accumulate we will be able to examine whether specific comorbid conditions alter the effectiveness of CBMPs for primary conditions such as chronic pain.
Depression is the leading cause of disability worldwide, contributing to the global disease burden. It can impair the quality of life of the individual and shorten life expectancy.
Major Depressive Disorder (Depression) was added as a primary condition in February 2022 when T21 opened up its eligibility criteria to cover all conditions for which medical cannabis can be prescribed. 72 individuals reported Depression as a primary condition and 1186 as a secondary co-morbid condition. The characteristics of these people are compared with those of T21 patients overall in the table below.
Contrary to existing literature*, Depression was more common amongst males (2.6%) compared to females (1.2%).

We measure mood and depression with a questionnaire called PHQ-9. This questionnaire goes out to all patients on T21, as depressed mood is common among people with chronic conditions.

Patients with a primary condition of Depression experience worse mood at baseline when compared with all other T21 patients. Patients from both groups experience a significant (p<0.05) improvement in mood/depression levels after 3 months, and the improvement is sustained at 6 months.
* Albert, P.R. (2015) ‘Why is depression more prevalent in women?’, Journal of Psychiatry and Neuroscience, 40(4), pp. 219–221. doi:10.1503/jpn.150205.
Post-traumatic stress disorder (PTSD) is a disorder that develops in some people after exposure to a traumatic event. People with PTSD often relive the traumatic event through nightmares and flashbacks, and may experience feelings of isolation, irritability and changes in reactivity.
As of April 2023 there were 221 patients with a primary condition of PTSD and 415 patients who reported it as a secondary condition. Of these 221 patients 59 had available data for baseline as well as 3 and 6 month follow-up. The below analyses are performed on those 59 people.
Patients with PTSD complete the PTSD CheckList – Civilian Version (PCL-C) which consists of 17 items corresponding to key symptoms of PTSD. Respondents rate how much they have been bothered by a symptom over the past month using a scale ranging from 1 (not at all) to 5 (extremely).
The PCL-C can be analysed in two ways. All items can be added up for a total severity score as in Figure 1 (range 17-85). Scores below 29 indicate little to no severity. Scores of 28-29 indicate some PTSD symptoms, while 30-44 indicate moderate to moderate high severity of PTSD symptoms and finally, scores between 45-85 indicate high severity of PTSD symptoms.
Figure 1 below shows the average PTSD symptom severity score over time for patients with a primary diagnosis of PTSD.

This scale can also be analysed by treating responses to individual items above 3 (moderately and above) as symptomatic, while responses between 1-2 (below moderately) are treated as non-symptomatic. A diagnosis of likely PTSD would require at least one symptomatic response to questions 1-5 (cluster B) corresponding to reexperiencing the trauma, at least 3 symptomatic responses to questions 6-12 (cluster C) corresponding to avoidance and at least 2 symptomatic responses to questions 13-17 corresponding to mood and arousal.
Figure 2 below shows that there was a steady decline in the number of people who responded positively (symptomatic) to one or more items in each symptom category (cluster). The number of people who met the criteria for a probable diagnosis of PTSD at the time the questionnaire was completed was significantly* reduced between baseline and 3 months and this reduction was sustained at 6 months**.
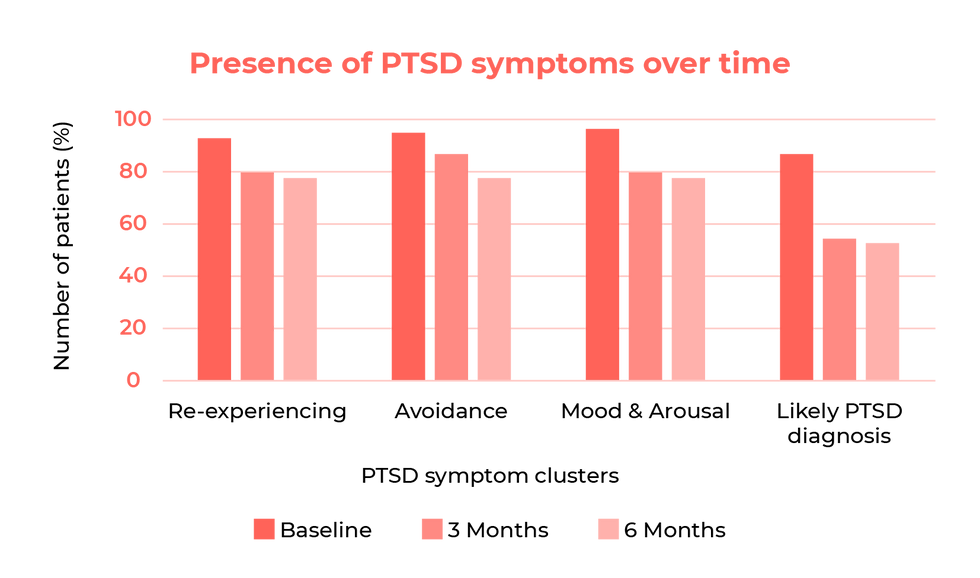
PTSD is one of the most commonly reported primary diagnoses and our evidence indicates that patients with PTSD experience reductions in symptomatology after receiving a CBMP prescription.
*p<0.05
** The percentage of people who meet a likely diagnosis of PTSD was 86% rather than 100%. This could be related to fluctuations in symptom severity over time, i.e. patient’s PTSD symptoms might get worse if they are going through a particularly stressful time. PTSD is a chronic condition and a degree of variation in symptom severity is expected. Additionally, errors in reporting or the reliability/validity of the screening instrument used might also contribute to these inconsistencies.In December2022 we looked at T21 patients’ prior experience with cannabis – you can read more about this here. Expanding on this analysis we wanted to explore the products that patients with different prior experiences with cannabis were prescribed at their initial consultation, i.e. first medical cannabis prescription. For the purposes of this analysis the following terms are defined as:
-
“Current daily users”: currently using cannabis daily or multiple times a day a (61.9% of the sample)
-
“Current non-daily users”: currently using cannabis less than daily (10.8% of the sample)
-
“Past or never users”: not currently using cannabis at baseline (27.3% of the sample)
Data on prescription and medical status at baseline was available for 3121 patients and can be seen in the table below.

The most commonly prescribed category of products across all patient groups was high THC flower with 59.4% of all patients being prescribed at least one strain of high THC flower. A higher percentage (72.3%) of current daily users were prescribed at least one high THC flower compared to 63.6% of current non-daily users and 48% past or never users.
Balanced oil was more commonly prescribed to past or never users (47.1%) compared to current daily (20.2%) or non-daily (26.3%) users.
Cannabis naïve (never users) or past users were prescribed high CBD oil more often (14.4%) than current non-daily (7.1%) and daily (4.1%) users.
As the project moves forward we will continue to explore the categories of products that patients are prescribed and track how these change over time.-
Although medical cannabis has been legal in the UK for more than four years, there still exists a great deal of stigma and resistance to medical cannabis among many people including health care providers.
Louise was diagnosed with osteoarthritis at the age of 21, diagnosed with fibromyalgia in her 40s and very recently diagnosed with Ehlers-Danlos syndrome (EDS) in her late 50s. She has been a medical cannabis patient for the past three years, joining T21 in June 2021. She had already undertaken multiple surgeries due to her conditions. In November 2022, she had two further surgeries, both on the same day: bone was harvested from her iliac crest before undergoing a cervical discectomy on two levels using her own bone to implant.
Louise did not want to take any pharmacological medications after surgery; rather she wanted to be in charge of her own health, and so preferred to use medical cannabis to handle post-operative pain. The clinician at her medical cannabis clinic wrote a letter to the private hospital and attached evidence of the prescription. The hospital reviewed the documentation, contacted the anaesthetist and surgeon to obtain their approval, and allowed Louise to consume her medication at the hospital as requested. When Louise arrived, they put her medication on a tray labelled with her details and stored it in the same way as medications that other patients had brought with them. Louise commented:
“They are making all reasonable adjustments for me and I’m delighted. I am very lucky; I have a great anaesthetist and surgeon!”

The first photo was taken in April 2021 when Louise weighed only 6 stone, and the second in January 2023 after three surgeries in 15 months, where Louise weighed 7 stone 10.
After the surgery, she was able to use an empty room nearby to vape her cannabis medication as needed. Patients who undertake this surgery are usually given opioids including Vicodin or Percocet which can have multiple side effects including drowsiness and light-headedness. Louise, however, was able to leave hospital after major surgery having needed only IV paracetamol and medical cannabis. Louise commented: “I would love for any medical cannabis patient to be able to use their medicine while at the hospital. I would like it to become more widely known that it can be done. Hospitals can accommodate this quite easily; all they have to do is let you bring your own medicine and let you vape or consume it.”
Ultimately, we hope that education and research will help destigmatise therapeutic cannabis among health care professionals and improve acceptance of and access to these medications in all settings, including hospitals. Positive experiences like this give us hope.
If you’re a T21 patient and would like to share your experience with us as a full case study, please do get in touch.
Fibromyalgia, also known as Fibromyalgia Syndrome (FMS), is a long-term condition that causes widespread pain and tenderness on touch. Fibromyalgia has a high female predominance, with females being more likely to have Fibromyalgia with a ratio of 9:1 . The condition typically develops between the age of 25 and 55.
Symptoms of Fibromyalgia can include increased sensitivity to pain, muscle stiffness, difficulty getting to sleep or staying asleep (fatigue), difficulty concentrating or remembering (fibro-fog), headaches, Irritable Bowel Syndrome (IBS), anxiety and low mood.
Symptoms can suddenly improve or get worse. Treatment can ease some of the symptoms, although they’re unlikely to disappear completely.
In T21, 113 people had Fibromyalgia as a primary condition (540 overall) and the characteristics of these people are compared with those of other chronic pain patients in the Table below. Consistent with existing literature, Fibromyalgia was found to be much more common in women (56.8%) than in men (40.5%) despite the fact that 2/3 of T21 patients are male.

Sleep outcomes are influenced by the primary condition of the patient with Fibromyalgia patients seeing greater improvement in sleep than chronic pain patients at 3 month follow up (p<0.05).

Patients with chronic pain experience higher levels of pain at baseline than Fibromyaligia patients. Both chronic pain patients and Fibromyalgia patients show similar and significant reduction in pain severity after 3 and 6 months of medical cannabis treatment.
[1] Yunus, M. B. (2001). The role of gender in fibromyalgia syndrome. Current Rheumatology Reports, 3(2), 128–134. https://doi.org/10.1007/s11926-001-0008-3
T21 patients are asked to complete some questionnaires describing their primary medical condition and general health at the start of their treatment and quarterly after that. Comparing scores at follow-up appointments to those at baseline helps us track patients’ progress and symptom management during their medical cannabis treatment. Up until now we have reported outcomes at baseline and 3-month follow-up. This month we have looked at longer term outcomes for the first time.
We measure quality of life using a well-validated questionnaire (EQ-5D-5L) where higher scores indicate worse quality of life. The figure below shows quality of life outcomes for 803 patients who had completed their baseline assessment as well as 3, 6 and 9 month follow-ups.
At 3 month follow-up, the mean rating on this scale was 11.0, indicating substantial improvement after only three months of being prescribed medical cannabis. Initial benefits are sustained in the long term as much as 9 months after initiation of treatment.
General health is measured using a simple visual analogue scale (VAS) which asks patients to assess on a scale of 0 to 100 how good or bad their health is today, with higher scores indicating better health. The figure below shows general health outcomes for 803 patients who had completed their baseline assessment as well as 3, 6 and 9 month follow-ups.
General health at baseline was 50. After 3 months of medical cannabis treatment the score increased to an average of 60 which was maintained at 6 and 9 months.
Our analysis shows that medical cannabis can be an effective medication for managing chronic conditions with initial benefits maintained in the longer term.
Future work will examine predictors of stability and change in symptom profiles across time.The initial evaluation (when a patient first joins T21) includes questions looking at whether the patient has ever used cannabis, whether they are currently using cannabis and whether their use is with the intention of treating their medical condition(s).
Unsurprisingly, only 11.2% of T21 patients had never tried cannabis at sign up. This might be caused by the lack of knowledge around the legality of medical cannabis, meaning that cannabis users might be better informed than the general UK population. Perhaps stigma also plays a role in preventing more cannabis-naïve patients from trying medical cannabis as a treatment option.
A majority of those who had ever used cannabis (72.8%) were currently using it at follow up. Of these, 85.2% reported using cannabis at least daily. The rest of the patients reported using it a few times a week (12.6%) or weekly (2.1%). Almost all current cannabis users (97.6%) reported using it with the intention of treating their medical condition(s). For the purposes of this analysis we will define medical users as “currently using cannabis daily or multiple times a day for medical purposes”. By this definition, 55.3% of the sample were classified as daily medicinal cannabis users. Non-daily users (44.7) included those who had never tried cannabis, past users and those using at baseline but infrequently.
There were significant* differences in the prevalence of different primary conditions between medical users and those not using cannabis medicinally when they commenced treatment. Chronic pain and psychiatric conditions were equally common amongst daily users, while for non-daily users, chronic pain was the most common condition with patients having substantially less likely to have psychiatric conditions.

Average baseline scores of daily medical users and non-daily users

As can be seen in the above table, there were small differences in the mean scores between daily medical users and non-daily users at the start of treatment. While daily medical users and non-daily users experienced similar levels of mood and sleep problems, non-users reported slightly worse quality of life and general health.
Average change between baseline and 3-month follow-up data between daily medical users vs non-daily users at baseline

Both groups experienced substantial improvements between baseline and three months. Non-daily users experienced a greater improvement in sleep. No other significant differences were found in the extent of improvement from baseline to three months between daily users and non-daily users.
These results were unexpected, as we would have anticipated that there would have been larger differences in 3-month outcomes between users and non-users. Possible reasons for the relatively high levels of improvement among people who are already using cannabis medicinally at entry to treatment include the potential difference between cannabis that can be procured illicitly and medical cannabis.
Additionally, perhaps cannabis naïve patients experience smaller improvement in the first 3 months due to titration of dosage and trialling of products, whereas daily users at baseline might have already experienced a substantial improvement in their symptoms so their rate of improvement might be slower.
Finally, perhaps the 3 month period does not allow adequate time for changes to appear, which is why subsequent follow ups are important. In a future data nugget we will be exploring whether trajectories of symptom change past 3 months will vary between prior users and non-users.
*X2=51.3, P<0.01
Attention deficit hyperactivity disorder (ADHD) is a common disorder that affects people’s behaviour. Although it is most frequently diagnosed during the school years, it affects individuals across the lifespan. People with ADHD can seem restless, may have trouble concentrating and may act on impulse. People with ADHD may also have additional problems, such as sleep and anxiety disorders .
We added ADHD to our list of conditions in December 2021 and we now have a big enough sample to be able to take a closer look at it.
-
101 (3.3%) patients have reported ADHD as a primary condition (1.4% of women, 4.2% of men, 9.4% of non-binary)
-
308 patients (10%) have reported it as a secondary condition
-
Insomnia is slightly less common amongst people with ADHD (23.8%) than the rest of the T21 sample (26.4%) though the difference is not statistically significantNS
-
There is a significant* comorbidity between ADHD and anxiety disorders. Secondary anxiety disorders are more common in patients with ADHD (68.3%) than the rest of the T21 sample with a primary condition other than an anxiety condition (40.6%)
-
The average general health score of patients with ADHD is 60.8 which is considerably lower than the previously estimated normative value for the United Kingdom population at 85.7 but better than the average of 49.8 of the rest of T21 patients.
-
People with ADHD have a smaller average number of pharmacological interventions that our other T21 patients which can perhaps be attributed to fewer treatment options being available for ADHD than for pain, for example.

People with ADHD appear on average healthier than other T21 patients but still experience problems, as seen from their outcome scores. There are relatively few treatments available for ADHD at the moment, but in the future, we’ll be able to explore whether cannabis is a good treatment option.
[1] https://www.nhs.uk/conditions/attention-deficit-hyperactivity-disorder-adhd/
[1] Jansen MF, Bonsel GJ, Luo N (2018) Is EQ-5D-5L better than EQ5D-5L? A head-to-head comparison of descriptive systems and value sets from seven countries. Pharmacoeconomics 36(6):675–697
* p<0.01
-
A year ago, in our October 2021 data nugget we explored pain in our T21 patients. This month we are expanding upon our analysis.
Patients with a primary condition that causes chronic pain are asked to complete the brief pain inventory form, a questionnaire which allows patients to rate the severity of their pain and the degree to which their pain interferers with daily activities. It includes 10 items which are rated from 0-10, with larger number indicating worse pain/interference.
Here are our findings…

1605 patients completed the Brief Pain Inventory (BPI) at baseline (when joining the study), recording an average of 5.9 for pain severity and an average of 7.0 for pain interference. At 3 month follow-up, based on 898 patients, these scores had dropped to 4.9 and 5.7 respectively. This drop indicates a statistically significant* decrease in pain levels after 3 months of medical cannabis treatment. The improvements in BPI scores were similar across gender and primary condition, whilst older patients benefited from a significantly** higher improvement.
*T=18.6, df=898, p<0.001
**b= 0.009, (0.004), p<0.01Sleep is vital for good health. People with chronic conditions often experience poor sleep. Through Twenty21, we measure the impact of medical cannabis on specific symptoms associated with both primary condition and quality of life – these include sleep.
The quality of sleep is measured by 4 simple questions which are rated from 1-5, with higher scores indicating more issues/interference with daily life, in addition to asking patients whether they experience insomnia.

As well as helping ameliorate symptoms associated with specific disorders, medicinal cannabis may also help improve other areas of life, including the quality of sleep. These improvements in sleep were similar across gender, age and primary condition.
At each follow-up appointment, we ask T21 patients to describe their condition-specific symptoms and other aspects of general health. Comparing these with reports (collected using the same questionnaires) at the start of treatment helps us to understand whether or not a patient’s health improves after they are first prescribed medical cannabis, and if so, by how much.
We also ask people to complete the Global Impression of Change Scale – this asks people to describe the change in activity limitations, symptoms, emotions and overall quality of life since starting treatment.

These results mirror those we have previously reported for improvements in anxiety symptoms (February, 2022 update), PTSD symptoms (January, 2022 update), mood (November, 2021 update) and anxiety/depression.
Together, this evidence indicates that people are experiencing substantial benefits from prescribed cannabis.
Ehlers-Danlos syndromes (EDS) are a group of rare inherited conditions (affecting 1 in 3,500-5,000) that affect connective tissue, primarily the skin, joints and blood vessel walls. People who have Ehlers-Danlos syndrome usually have overly flexible joints which can cause joint pain and frequent dislocations and stretchy, fragile skin that does not heal well, leaving gaping scars. Symptom severity can vary from person to person and depends on the specific type of EDS that a person has. There are 13 types of EDS, with the most common being Hypermobile EDS (hEDS). At the moment, there is no known cure for EDS – but there are treatments for the symptoms which include pain.

EDS is more prevalent in women than in men, despite the fact that 2/3 of T21 patients are male. This is consistent with the findings from a Welsh study of everyone diagnosed with EDS where 70% of the sample was female. EDS patients are slightly younger on average than T21 patients overall. They report a significantly higher number of secondary conditions,* but when it comes to health outcomes, EDS patients reported similar levels of average general health as well as pain interference and severity to that of other chronic pain patients.
It is our hope that, as we gather more data, we will see a significant improvement in these patients’ outcomes, including their pain and overall quality of life, and a decrease in the number of medications they need to use in addition to their medical cannabis prescription.

Multiple Sclerosis (MS) is an autoimmune disease of the brain and spinal cord affecting the central nervous system. This lifelong condition can cause serious disability and currently there is no cure. However, there are treatments that aid recovery from attacks by modifying the course of the disease and managing symptoms.
Currently on the NHS there is only one medically approved cannabis-based treatment available for MS – Sativex. This is an oromucosal spray containing 27mg of THC and 25mg of CBD per ml. Sativex is the only drug in the UK with a license to treat muscle stiffness and spasms (spasticity) caused by MS. But it doesn’t work for everyone.
Back in 2014, 1 in 5 people with MS surveyed by the MS Society said they had used cannabis to help with their symptoms, including muscle spasms or stiffness and pain. A 2019 paper showed that cannabis use is more prevalent in people living with MS, again suggesting that cannabis might be beneficial. Although Sativex is the only cannabis-based medicine approved for use on the NHS, patients can access a range of whole plant cannabis flower and oil products through Project Twenty21.
Project Twenty21 opened up its eligibility criteria to cover all conditions for which medical cannabis can be prescribed in February this year. The change has allowed us to look more closely at the types of anxiety conditions patients are reporting and the types of conditions that cause chronic pain. From here, we will be able to examine whether different forms of anxiety or pain respond better or worse to cannabis-based medicines (CBPMs) as well as what specific treatments may be optimal for different types of anxiety or pain.
The most commonly reported chronic pain condition among those selecting a specific chronic pain condition since the eligibility update (168) is back and/or neck pain at 27%, followed by fibromyalgia (19%) and arthritis (13%). These three conditions combined make up 59% of all patients who reported a specific chronic pain condition.

The most commonly reported anxiety condition among those selecting a specific anxiety condition since the eligibility update (39) is generalised anxiety disorder at 56%, followed by social anxiety disorder (21%) and agoraphobia (8%). These 3 conditions combined make up 85% of all patients who reported a specific anxiety condition.

Based on our current data (2633 patients) the most common individual condition on Project Twenty21 since the beginning of the project is PTSD at 25.7%, followed by Multiple Sclerosis (12.5%) and ADHD (10.4%). Chronic pain and anxiety still make up the largest proportion of our patients, however these are condition clusters and not individual conditions.

Using a snapshot from one of our previous data sets, we have been able to show in the below map that our Project Twenty21 patients are based all over the UK – as far north as the Shetland Islands, right down to the foot of Cornwall.
Our medical cannabis patients, whose age currently ranges from 18 to 96 years old, are not focused only in metropolitan areas but are geographically very spread out, which suggests a diverse and varied group of people. These are people from all walks of life, which only serves to demonstrate further why cannabis-based medicines should be made available for everyone to access on the NHS.
The most commonly reported anxiety condition among those selecting a specific anxiety condition since the eligibility update (39) is generalised anxiety disorder at 56%, followed by social anxiety disorder (21%) and agoraphobia (8%). These 3 conditions combined make up 85% of all patients who reported a specific anxiety condition.


Post-Traumatic Stress Disorder (PTSD) is a mental health condition that can develop after exposure to any traumatic event. Symptoms include re-experiencing the trauma (e.g., nightmares, flashbacks), avoidance of trauma related stimuli, cognitive and mood changes and alterations in arousal and reactivity (e.g., irritability, difficulties concentrating).
It is relatively common in the general population with estimates suggesting that 5-10% of the general population may experience PTSD in their lifetime while some groups (e., war veterans) have heightened rates of this condition.
Some anecdotal and observational studies some studies indicate that prescribed cannabis is a promising treatment for PTSD. But the quality of this evidence has been judged low and potentially subject to bias.
So, when it comes to the judging the safety and efficacy of cannabinoids for the treatment of PTSD, there is a need for high quality data.

Chronic Pain totals more than half of all patients on the study, with Anxiety coming up second – this reflects what we see more widely at present with medical cannabis patients in the UK. As pain encapsulates so many conditions, it is unsurprising that we see the largest number of patients in this category, and we’re keen for a more in-depth analysis of the conditions it covers.
And so, we are excited to announce an update to our eligibility criteria. In the new year, you can join the study if you have any diagnosed condition that can be treated with medical cannabis at one of our participating clinics, providing you meet the clinic’s eligibility criteria.
Not only will this help us gain better insight into specific pain conditions experienced by patients, it will also enable more people to access medical cannabis through Project Twenty21.A closer look at how and why we analyse the mood of patients enrolled with Project Twenty21…

So far with our monthly data nuggets, we’ve covered sleep, anxiety and trends within our youngest 18-25 group for the project. This month, we’re delving deeper into chronic pain…

Patients with Project Twenty21 range from 18 to 80+ years old, but only 10% of patients fall into the youngest 18-25 age bracket…

Every 3 months, we ask patients to fill in questionnaires, which vary according to a patient’s primary condition, in exchange for being able to benefit from subsidised medical cannabis products from our partners. This is how we collect our data for Project Twenty21, so it’s vital that patients submit this information in order for T21 to operate.

Although sleep is not one of the primary qualifying conditions for T21, we are finding that it affects many patients with the disorders we’re studying. Our baseline data shows that many of this patient group experienced substantial difficulties with sleep, and follow-up analyses will examine whether prescribed cannabis improves sleep.










.jpg)